Health professionals
People need and expect clear advice
Women who are pregnant or trying to conceive need and expect clear advice on substances that can harm their pregnancy and developing baby – like alcohol.
One in seven women drink alcohol after becoming aware of their pregnancy1 and one in four who are pregnant or would consider having a baby soon, are unaware that drinking alcohol during pregnancy can cause Fetal Alcohol Spectrum Disorder (FASD)2.
Health professionals play an important role in providing clear and accurate information and advice about how to have a healthy pregnancy.

Looking for training?
Update your knowledge and skills with our eLearning course, Supporting alcohol-free pregnancy and safe breastfeeding. It’s free and accredited by the Royal Australian College of General Practitioners (RACGP), the Australian College of Midwives (ACM), the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) and the Australian College of Rural and Remote Medicine (ACRRM).

The moments you spend with her matter
This includes making it routine practice to ask about alcohol, assessing use with a validated tool, and providing advice and support based on the level of risk.
As one of the most trusted sources of information on pregnancy, health professionals are vital in communicating the updated National Health and Medical Research Council’s (NHMRC) Australian guidelines to reduce health risks from drinking alcohol, which advise:
- women who are pregnant or planning a pregnancy should not drink alcohol.
- for women who are breastfeeding, not drinking alcohol is safest for their baby.
Looking for
more information?
Browse resources for health professionals, including topic guides and evidence briefs.
Find specialist AOD services for people who are pregnant.

Facts at a glance
Common questions
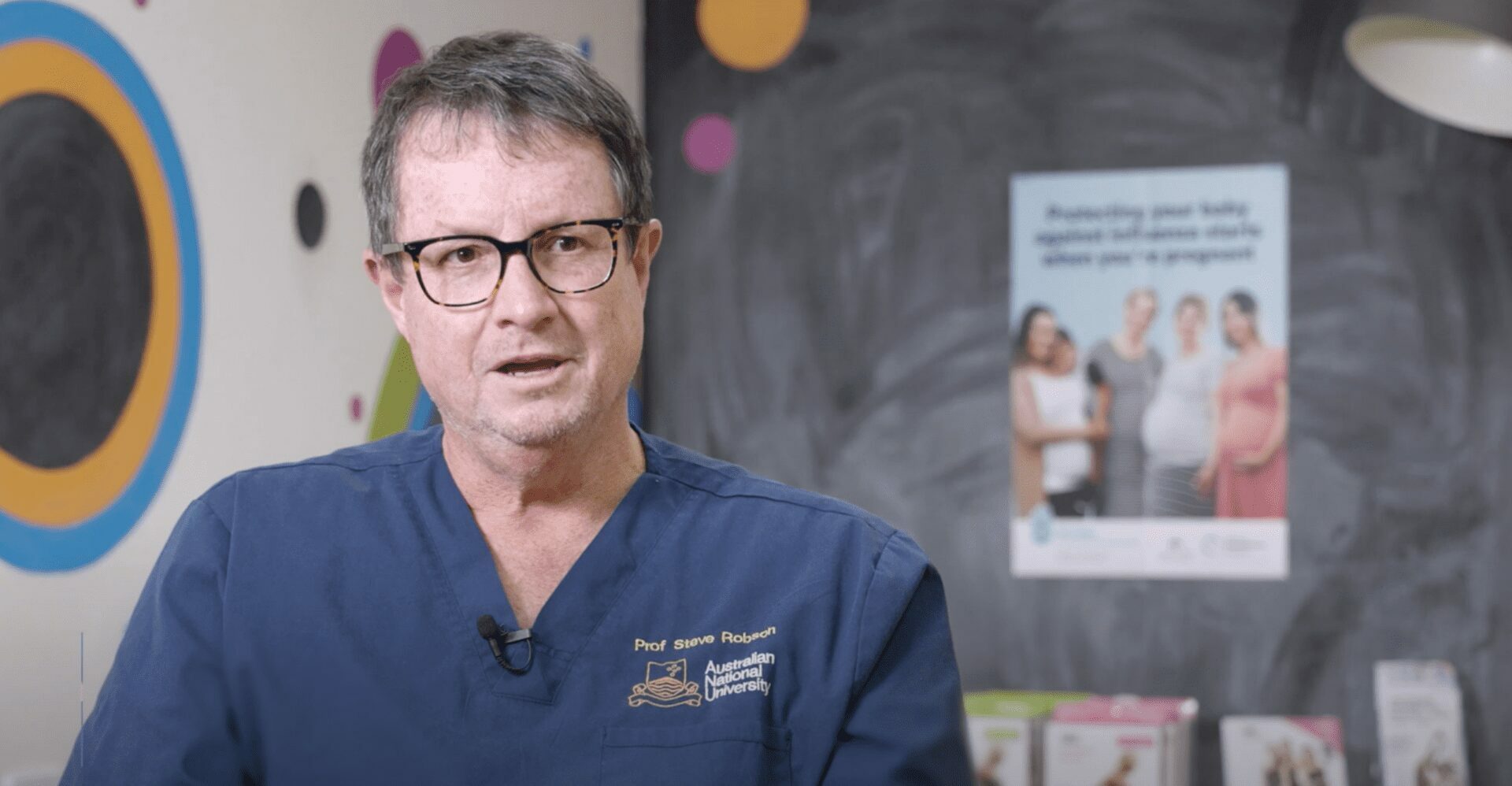
Perspectives from health professionals
References
- Australian Institute of Health and Welfare. 2020. National Drug Strategy Household survey 2019. https://www.aihw.gov.au/reports/illicit-use-of-drugs/national-drug-strategy-household-survey-2019/contents/summary
- Kantar Public. 2021. Alcohol and pregnancy. Research conducted by Kantar Public on behalf of the Foundation for Alcohol Research and Education. https://fare.org.au/wp-content/uploads/263406881_Alcohol-and-pregnancy-Topline-report_FINAL-1.pdf
- National Health and Medical Research Council. 2020. Australian Guidelines to Reduce Health Risks from Drinking Alcohol. Commonwealth of Australia. Canberra.
- Bailey, B.A. & Sokol, R.J. 2011. Prenatal alcohol exposure and miscarriage, stillbirth, preterm delivery and sudden infant death syndrome. Alcohol Research & Health. 34(1) 86-91
- Patra, J., Bakker, R., Irving, H. et al. 2011. Dose-response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age. A systematic review and meta-analyses. BJOG. 188. 1411-21
- Aliya, M.H., Wilson, R.E., Zoorob R. et al. 2008. Alcohol consumption during pregnancy and the risk of early stillbirth among singletons. Alcohol. 42(5) 369-374.
- Caputo, C., Wood, E. & Jabbour, L. 2016. Impact of fetal alcohol exposure on body systems: A systematic review. Birth defects research part C. Embryo Today 108(2) 174-80
- Mattson, S.N., Bernes, G.A. & Doyle, L.R. 2019. Fetal alcohol spectrum disorders: A review of the neurobehavioural deficits associated with prenatal alcohol exposure. Alcohol Clin Exp Res. 43(6) 1046-1062
- O’Leary, C.M., Bower, C., Zubrick S.R. et al 2010. A new method of prenatal alcohol classification accounting for dose, pattern and timing of exposure. Journal of Epidemiology & Community Health. 64:956-962
- Bower, C. and Elliott, E.J. 2016. On behalf of the Steering Group. Report to the Australian Government Department of Health: Australian Guide to the diagnosis of Fetal Alcohol Spectrum Disorder (FASD). https://www.fasdhub.org.au/fasd-information/assessment-and-diagnosis/guide-to-diagnosis/